phone | 702-228-7355

phone | 702-228-7355

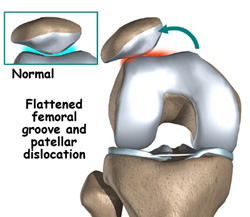
Patients who have problems with the kneecap (patella) can have pain around the front of the knee and/or episodes of the patella slipping out of the groove (trochlea) where it belongs (patellar instability). When the patella comes all the way out of the groove that is called a patellar dislocation. Sometimes the patella goes back in place spontaneously, but sometimes it must be pushed back in place either by the patient or another person, sometimes requiring a trip to the emergency room.
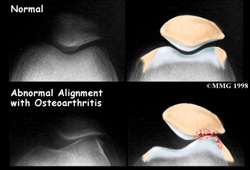
Anterior knee pain is often the result of patellofemoral problems. Patellofemoral malalignment can result from a acute injury such as a patellar dislocation or acute subluxation or it may develop gradually in patients who are predisposed. Anterior knee pain can also result from overuse of a "normal knee." Normally the patella (knee cap) glides smoothly into its grove (trochlea). It is very important to have excellent muscle strength and control to help guide the patella during activities. Tightness or lack of flexibility can cause the patella to track incorrectly through the trochlea or to overload tissues to the point of causing pain. When the patella tracks abnormally, stress is concentrated in the bone and surrounding soft tissues and pain often results. The majority of the time such malalignment can be successfully treated by an exercise program which includes stretching the tight structures and strengthening the muscles which have become relatively weak. When pure overuse is a major part of the problem, activity limitation is a necessary part of the treatment. When this fails to produce adequate improvement and patellofemoral malalignment can be documented by studies such as a CT scan, patellofemoral realignment surgery can often produce significant pain relief.
Some patients with patellofemoral instability (patellar dislocation or subluxations, that is, partial dislocation) have persistent pain or episodes of instability and would benefit from patellofemoral realignment. Many patients with patellar instability do not need surgery. Some do. A complete and dedicated rehabilitation program is essential before committing to surgical treatment.
Depending on the degree of malalignment present, the surgery which is necessary can be as simple as cutting the tight lateral retinaculum which holds the patella in a laterally tilted position. In some patients this can be accomplished arthroscopically. This surgery is usually done as outpatient surgery. After such a procedure there is a period of exercise and rehabilitation during which it is critical for the patient to begin early motion and strengthening of their leg.
In some patients with patellar instability without severe damage to the cartilage surface of the patella, an operation to balance the medial and lateral ligaments which guide patellar tracking can be very successful. This may include imbrication (tightening) or reconstruction (using a graft to rebuild) of the medial ligaments and at times release or lengthening of the lateral retinaculum.
Patients who have more severe malalignment and particularly those who have had recurrent patellar dislocations with damage to the cartilage surface of the patella are better treated by a realignment procedure which includes tibial tubercle transfer. This means that the bony attachment of the patellar tendon to the tibia is moved to ensure that the patella tracks more correctly. In cases where there is significant degenerative change of the patella, the tubercle is also shifted forward. This operation is combined with a lateral release to complete the realignment. The combination of these two procedures is referred to as anteromedialization of the tibialtubercle (AMZ).
Patellofemoral realignment operations are performed in the operating room under either a general or spinal anesthetic. Patients undergoing lateral release generally can be treated as out- patients. Many patients who have proximal realignment are successfully treated as outpatients. Patients undergoing the more extensive anteromedialization of the tibial tubercle (AMZ) are generally admitted for at least one night following their surgery. Most often patients are comfortable enough to go home the next day after AMZ. Exercises begin immediately after surgery in either case. Following patellofemoral realignment patients will usually be able to return to office type jobs or to class within one week after surgery.
Dedication to your exercise program after surgery is a critical portion of your treatment. It is very important that you be committed and dedicated to working hard at this portion of your treatment.
If you have any questions regarding your condition or the treatment options you face. Please do not hesitate to call and discuss this with me. I understand this is a very important decision for you and I urge you to understand both the facts regarding your condition and impact it will have on your life after your treatment. If you do elect to have me do your surgery, rest assured that I will work closely with you to achieve the best results possible.